Part 1: Neurodivergence, IBS and food reactions
Research is increasingly linking all types of health conditions to our digestive health, gut microbiota and nutrition, yet this is an area neurodivergent people can struggle with the most, many of us experiencing difficulties since early on in life.
We understand the importance of nutrition as a foundation to health, however whether we are able to absorb the nutrients and building blocks of our bodies eaten in our diet depends on our digestive capacity.
Understanding the Gut-Mental Health Connection
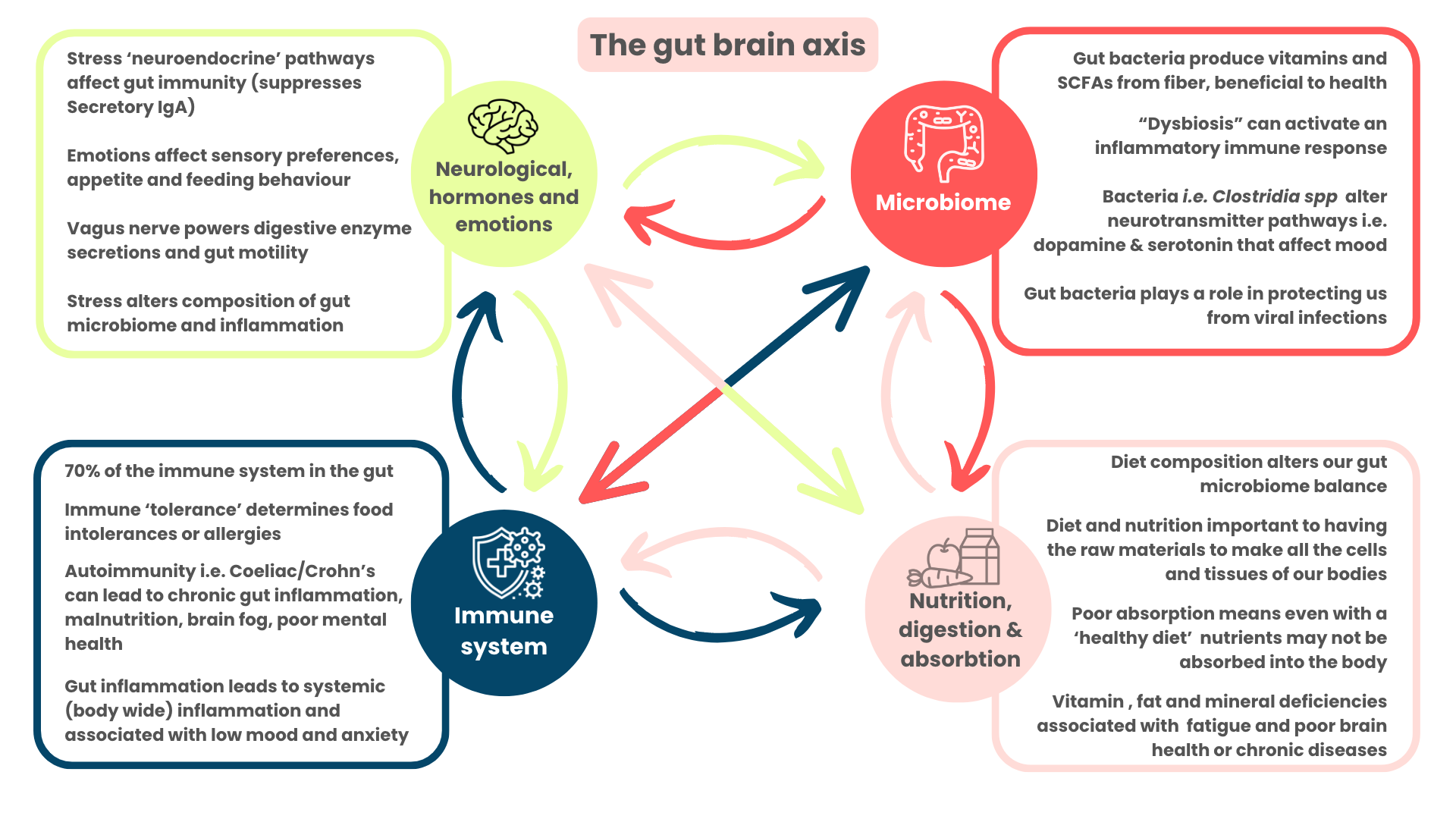
90% of our neurotransmitters are produced and held in the gut and research is showing this can directly and indirectly impact on our mental health and behaviour. The intestinal nervous system (mainly the vagus nerve) is a bi-directional communication superhighway that runs between the gut and the brain carrying information both ways allowing us to adapt and react dynamically.
Our gut-brain axis refers to the larger network that includes the nervous system, hormonal signalling, the microbiome and the immune system that interact together in complex ways to influence our physical wellbeing, our mental health and our longevity.
Our understanding of psychiatric conditions has expanded to include gut microbiome and immune imbalances as key drivers of anxiety and depression.
Studies have shown the association between chronic inflammation and mood disorders, with one potential source of inflammation being from our intestinal environment.
A study in Chronic fatigue syndrome administered lipopolysaccharide a type of toxin found in gut microbes into CFS patients with CFS/ME and found this increased levels of stress hormones (cortisol and epinephrine), higher anxiety, lower mood and elevated blood markers of inflammation. This relationship was dose-related.
Conversely microbiome profiles of CFS/ME and Long-COVID find lower levels of gut bacteria such as Bifidobacterium Ruminococcus genus faecalibacterium prauznitzii which produce anti-inflammatory chemicals, and these ‘altered profiles’ are linked to severity of illness and risk of developing chronic illness from a viral infection.
A 2022 review of 28 studies looked at the effects of fecal microbial transplantation - transferring gut bacteria from a healthy donor into people with a range of psychiatric illnesses found improvements in their conditions, at least in the short term.
The Neurodivergent-Gut Connection
Autistic and ADHD children and adults are more likely to suffer from digestive and gastro-intestinal problems including Irritable Bowel Syndrome and many types of food reactions. This vast number of overlapping symptoms can look very complex and it can become difficult for the person or their doctor or practitioner to tease out the root cause. This leaves treatment down to chance or long-term sticking bandaids over symptoms without addressing the underlying problem and this approach often leads to more related health issues later down the line.
Common gut and feeding difficulties that affect my neurodivergent patients:
Allergies, intolerances and interoceptive food reactions:
This makes up a diverse range of food reactions that patients that come to see me in clinic with. Frequently more than one type of reaction happens in the same person but the underlying cause is often connected.
Infections, inflammation and immunity:
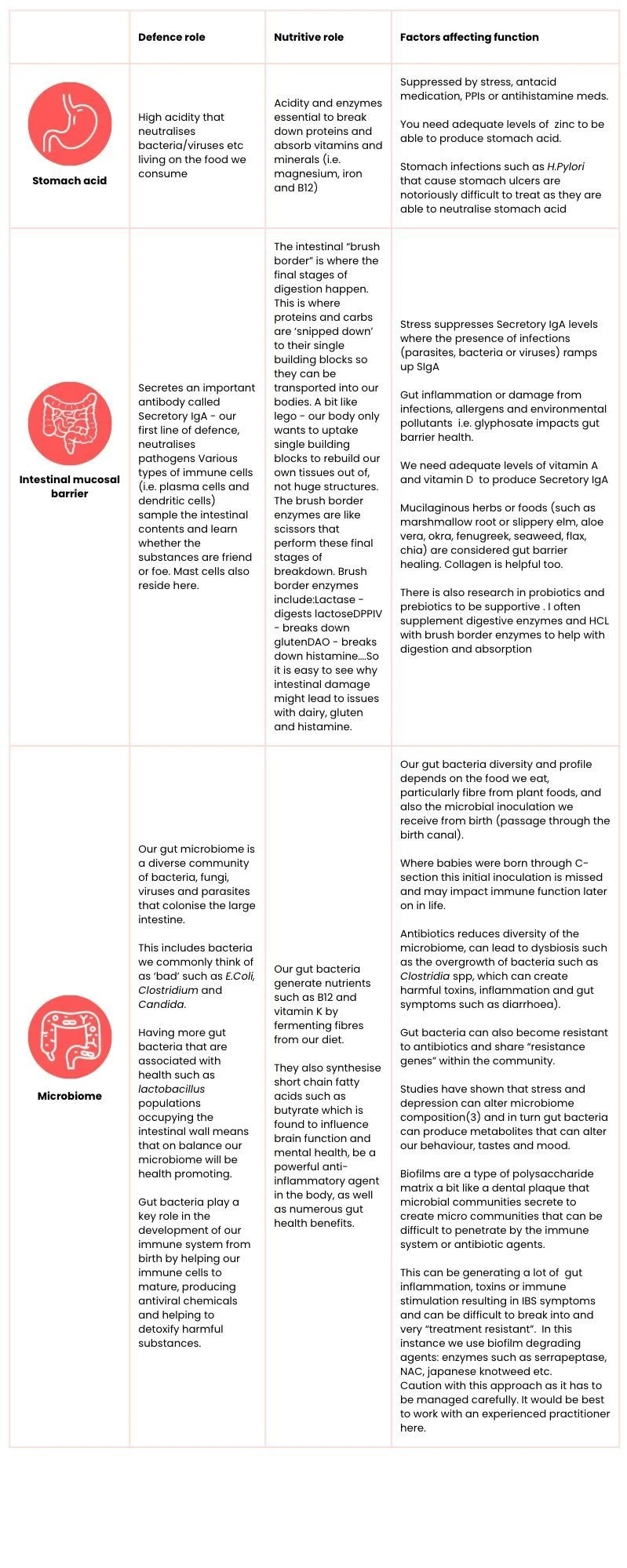
The gut hosts 70% of our immune system and is the place where our immune cells develop ‘immune tolerance’ - how to determine what is friend or foe.
Without a degree of tolerance, our immune system would react to absolutely everything, including harmless substances like food or even our own microbiome (which is what happens in people with multiple food and chemical reactions). With too much tolerance we would be vulnerable to pathogens and microbes entering our bodies undetected which could lead to serious or chronic infections (such as with Long-covid, CFS or pervasive gut infections such as SIBO).
I explain to my patients that the intestinal environment is technically still the ‘outside’ of the body as nothing has passed through the gut wall into our bloodstream yet. This includes the food we eat and supplements we take. Without good digestion and absorption it is entirely possible for food to be eaten and excreted without any nutrients entering our bodies.
Any bodily surface that interfaces with the ‘outside world’ needs a huge first line of defence to keep out harmful substances and microbes from entering our system, whilst allowing the entry of essential nutrients.
Our gut defence system is made up of:
Looking at the above criteria for healthy immune development and optimal nutritional intake, it is clear Autistic and ADHD individuals can have many challenges and barriers to achieving the best health possible.
Studies in gut health and Autistic children demonstrate dysbiosis, low microbial diversity, raised markers of gut inflammation, nutritional deficiencies and many other digestive issues that correlate with mood disorders and behaviours of distress(McElhanon et al, 2014)(Buie et al, 2010). However simply expanding the diet to include more diverse fibres can be inaccessible to Autistic people with sensory issues, or removing allergens and ‘simple swaps’ is especially hard for people who struggle with change or when these staples are a safe food for them.
In part 2- I delve into some of the common motor challenges I see in my patients and how I support all of this in an ND-affirming way.